Clinical Evidence
Explore the extensive body of clinical research examining the effectiveness, efficacy, and safety of Maggot Debridement Therapy (MDT). This section presents a comprehensive compilation of studies that shed light on the therapeutic benefits of MDT, providing valuable insights into its potential applications in healthcare. Scroll down to access the compelling evidence supporting the use of MDT in various clinical contexts.
MDT Has Been Clinically Proven to Be More Effective Than Conventional Treatment
Vs. Surgical Debridement
18x Faster Cleaning
Studies on Maggot Therapy for wound debridement have also shown that compared to the conventional method of using a scalpel or scissors, Maggot Therapy can clean wounds up to 18 times faster [1].
Vs. Negative Wound Pressure Therapy
5x Higher Healing Rate
Only 18.2% of patients undergoing NWPT had their wounds closed, whereas 92.3% of patients undergoing Maggot Therapy had their wounds closed, according to a randomised clinical trial [2]. NWPT is also known as Vacuum-Assisted Closure (VAC).
Vs. Hydrogels
5x Faster Debridement
Wounds treated with Maggot Therapy took only 14 days to debride, whereas wounds treated with hydrogels took 72 days, as observed by a randomised controlled clinical trial [3].
[1] Health Hub Singapore. [2] Cangel U, Sirekbasan S, Polat E. Comparison of Larval Therapy and Vacuum-Assisted Closure Therapy after Revascularization in Peripheral Artery Disease Patients with Ischemic Wounds. Evid Based Complement Alternat Med. 2022 Mar 29;2022:8148298. [3] Zarchi K, Jemec GB. The efficacy of maggot debridement therapy--a review of comparative clinical trials. Int Wound J. 2012 Oct;9(5):469-77. doi: 10.1111/j.1742-481X.2011.00919.
MDT is Safe
Maggot Debridement Therapy has proven to be a safe and effective method of debridement, with the pain resulting from MDT easy to manage.
A clinical paper studying the safety and efficacy of MDT using Lucilia cuprina reported that MDT had minimal side effects, besides discomfort. They reported that the mean visual analogue pain score was just 3.3 (Yeo et al., 2022).
Maggot Debridement Therapy is widely used globally. In Singapore, MEDIFLY is a registered under the Health Science Authority (HSA) as a Class C medical device and is widely used in both public and private hospitals. In the United States, the use of medicinal maggots was approved by Food and Drug Administration (FDA) as a medical device in 2004. MDT has been used in more than 30 countries in the world.
MDT is Affordable
MDT is more economical than conventional wound care therapy in all cost categories.
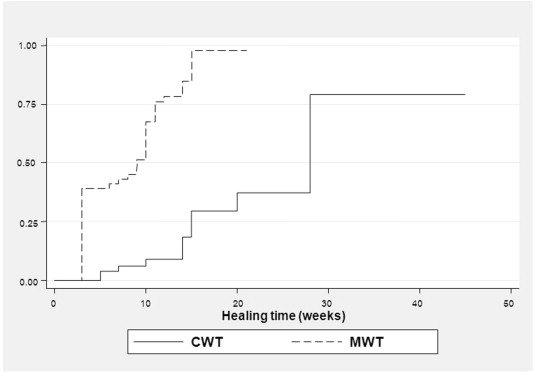
A Thailand-based study found that the average cost of MDT in patients with Diabetic Foot Ulcers (DFU) was more than 50% lower that of conventional therapy, with medians of US$292.82 and US$490, respectively. This cost saving is in part due to MDT’s shorter healing time (Wilasrusmee et al., 2014).
A United Kingdom study investigated the cost effectiveness of MDT compared to other types of chronic wound debridement and concluded that MDT was the most effective and less costly method considered. That is, adopting the use of MDT may result in both cost savings and greater benefits for a patient over one year (Bennett et al., 2013).
A Mexico-based study added that the cost of MDT is “much less” than the cost of surgery, which includes facilities, supplies, and personnel time (Fonseca-Muñoz, 2020).
Figure 6. Kaplan-Meier estimates of healing between maggot wound therapy (MWT) and conventional wound therapy (CWT) (Wilasrusmee et al., 2013).
“Adopting the use of MDT may result in both cost savings and greater benefits for a patient over one year.”
MDT Provides Effective Debridement of Necrotic Tissue vs. Conventional Therapy
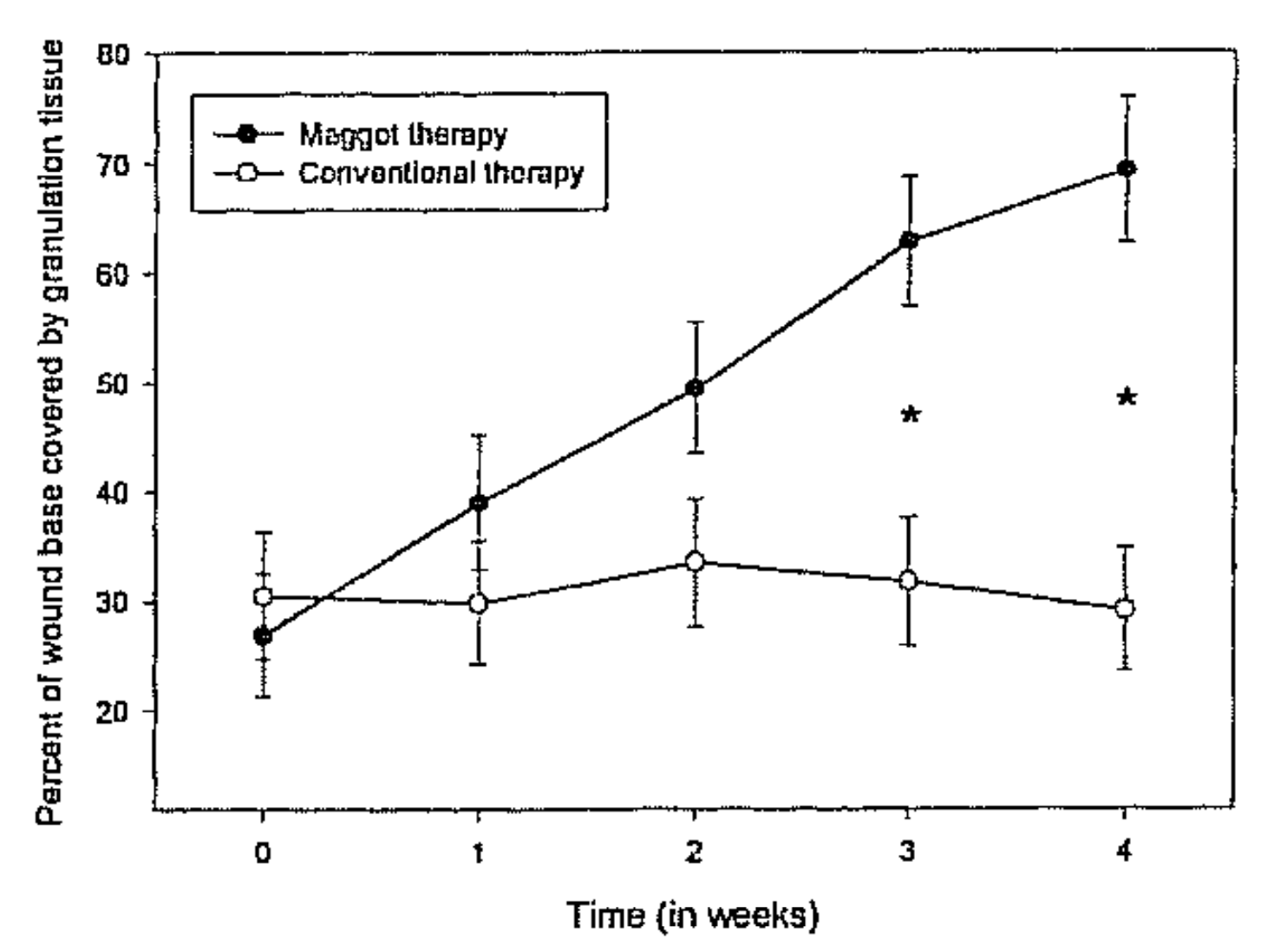
A clinical study found that Maggot Debridement Therapy was more effective and efficient in debriding nonhealing foot and leg ulcers in male diabetic veterans than was continued conventional care.
According to the study, during the first 14 days of conventional therapy, there was no significant debridement of necrotic tissue; during the same period with maggot therapy, necrotic tissue decreased by an average of 4.1 cm².
After five weeks of therapy, conventionally treated wounds were still covered with necrotic tissue over 33% of their surface, whereas after only four weeks of therapy, maggot-treated wounds were completely debrided (Sherman, 2003).
Another study reported on 25 patients suffering mostly from chronic leg ulcers and pressure sores in the lower sacral area. Underlying diseases were mainly venous ulcera (48%) and paraplegia (20%). Using maggot therapy, complete debridement was achieved in 38 wounds (88%). Importantly, In five patients who were referred for amputation of the leg, the extremities was salvaged after maggot therapy (Mumcuoglu et al., 1999).
Figure 1. Surface area of necrotic tissue over time, during treatment with maggots (•; n = 14) or standard therapy (○; n = 14). Six wounds received conventional therapy only, six received maggot therapy only, and eight received conventional therapy followed by maggot therapy. Error bars indicate standard error. *P < 0.05 (Sherman, 2003).
“After only 4 weeks of therapy maggot-treated wounds were completely debrided.”
MDT Provides Targeted Debridement for Chronic Wounds
Maggots perform debridement by physically feeding on dead tissue, cellular debris and exudate present in sloughy wounds. The feeding action physically breaks up necrotic or sloughy tissue, which is then consumed and digested.
This process is mediated by proteolytic enzymatic digestion through a process of extracorporeal digestion (Chambers et al., 2003). Collagenases, trypsin-like and chymotrypsin-like enzymes are secreted which breakdown devitalised tissue into a semiliquid form which the larvae can ingest (Hobson, 1931; Vistnes et al., 1981).
The maggots do not digest living human tissue, and they work without damaging viable tissue. This selective process is one of the major advantages of maggot debridement therapy as it spares the healthy tissues necessary for healing. (Nigam et al., 2006).
“Maggots debride wounds quickly and effectively, without damage to viable tissue.”
Figure 2. The mean percentage slough pre, during and post MDT (n=11). There was 45% reduction in slough following the 2nd cycle of MDT compared with baseline (p<0.001) (Yeo et al., 2022).
MDT Promotes Growth of Granulation Tissue
Studies have shown that Maggot Debridement Therapy hastens the growth of granulation tissue, signifying a progression of wound healing.
One study reported that MDT-treated wounds contained twice the granulation tissue compared to non-MDT-treated wounds. The average MDT-treated wound was covered 60% by healthy granulation tissue within three weeks (Sherman, 2002).
Another study reported that MDT-treated ulcers have about seven times higher chance of wound healing vs. conventional therapy (Wilasrusmee et al., 2014).
Additionally, MDT achieved significantly better granulation rates and shorter healing times than conventional therapy in pressure ulcers and diabetic foot ulcers (Shi et al., 2014).
Figure 3. Average percentage of wound base covered by granulation tissue during MDT (N=43) or conventional therapy only (N=49). Error bars indicate standard error; asterisks indicate significant differences in mean percentage of granulation tissue (p<0.05) (Sherman, 2002).
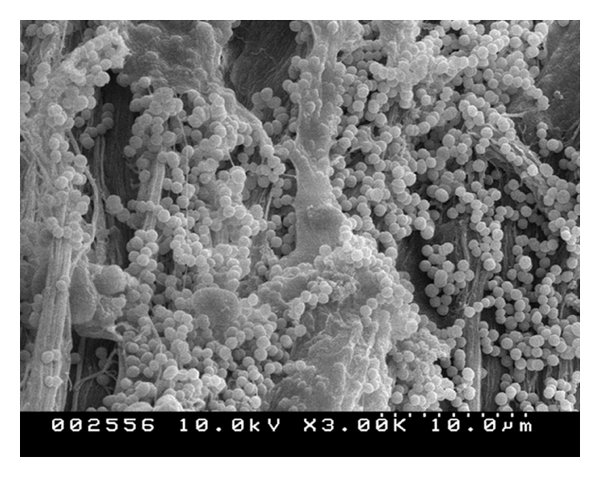
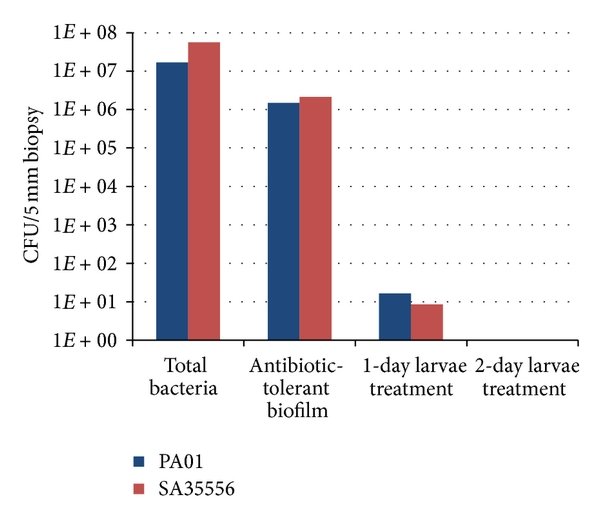
MDT Reduces and Prevents the Formation of Biofilm
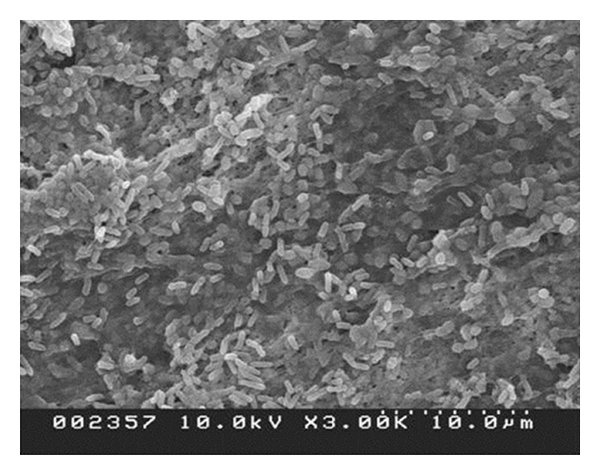
Biofilms can precipitate chronic inflammation and the failure of wounds to progress to healing (Davies et al., 2008). They do so by creating a favorable environment for bacterial growth by forming sessile communities encased in self-produced extracellular matrices (Pritchard et al., 2015).
MDT has been shown to be effective against biofilm formation, and at the same time, it is effective in the removal of biofilms (Cazander et al., 2008).
In a tissue biofilm model, a study demonstrated that maggots eradicated established S. aureus biofilm from experimental pigskin explants within 24 hours. The authors investigated many topical treatments, including negative pressure wound therapy (NPWT), as well as silver- or iodine-containing dressings with regard to antibiofilm action (Cowan et al., 2013).
“Biological debridement (with MDT) may be the only 100% effective topical antibiofilm strategy able to completely remove mature biofilm from pigskin explants within 24–48 hours.”
→
Figure 4.1. Three-day PA01 biofilm on pig explant (before maggots are applied) (Cowan et al., 2013).
Figure 4.2. PA01 biofilm on explant (24 hours after larvae are applied) (Cowan et al., 2013).
→
Figure 4.3. Three-day SA35556 biofilm on pig explant (before larvae are applied) (Cowan et al., 2013).
Figure 4.4. SA35556 biofilm on pig explants (24 hours after larvae are applied) (Cowan et al., 2013).
MDT Has Antimicrobial Effects
With regards to chronic wounds, bacterial infection can both compromise and delay wound healing (Roy et al., 2020). Progression of healing is said to be dependent on both bacterial count and the microbial species present, so managing the bacterial levels of the wound site is vital for healing (Negut et al., 2018).
Several studies have served to reaffirm the notion that maggot secretions are effective in destroying a broad range of gram-positive and gram-negative bacteria (Jaklic et al., 2008; Daeschlein et al., 2007).
In vitro evidence shows that Maggot Debridement Therapy supports the cleansing of the prepared wound bed. Maggots possess multiple antimicrobial strategies, with a putative small molecule and definitive peptide repertoire dealing with Gram-positive microbes in particular, and antibiofilm enzymes providing support in dealing with Gram-negative microbes such as P. aeruginosa (Pritchard et al., 2015).
The serine protease chymotrypsin 1 in maggots was shown to disrupt S. aureus biofilm (Harris et al., 2013), and maggot nuclease was demonstrated to digest extracellular bacterial DNA contained in matured P. aeruginosa biofilms (Brown et al., 2012).
In addition, maggots elevate the pH in wounds, which inhibit bacterial growth. This is because maggots secrete various alkaline compounds, such as ammonium carbonate, calcium, allantoin and urea (Parnés et al., 2007).
Infections cure faster, and patients remain infection-free for a longer period with MDT (Shi et al., 2014).
Figure 5. Graph of bacterial CFU (colony-forming unit) before and after maggot exposure (Cowan et al., 2013).